by Admin
California’s Primary Care Shortage Persists Despite Ambitious Moves To Close Gap
Sumana Reddy, a primary care physician, struggles on thin financial margins to run Acacia Family Medical Group, the small independent practice she founded 27 years ago in Salinas, a predominantly Latino city in an agricultural valley often called “the salad bowl of the world.” Reddy […]
Rural Health
by Admin
Federal Cuts Gut Food Banks as They Face Record Demand
Food bank shortages caused by high demand and cuts to federal aid programs have some residents of a small community that straddles Idaho and Nevada growing their own food to get by. For those living in Duck Valley, a reservation of about 1,000 people that […]
Health Care
by Admin
The Patient Expected a Free Checkup. The Bill Was $1,430.
Carmen Aiken of Chicago made an appointment for an annual physical exam in July 2023, planning to get checked out and complete some blood work. The appointment was at a family medicine practice run by University of Illinois Health. Aiken said the doctor recommended they […]
Health Care

‘If They Cut Too Much, People Will Die’: Health Coalition Pushes GOP on Medicaid Funding
by Admin
Tina Ewing-Wilson remembers the last time major Medicaid cuts slashed her budget. In the late 2000s, during the Great Recession, the pot of money she and other Medi-Cal recipients depend on to keep them out of costly residential care homes shrank. The only way she […]
Health CareTina Ewing-Wilson remembers the last time major Medicaid cuts slashed her budget.
In the late 2000s, during the Great Recession, the pot of money she and other Medi-Cal recipients depend on to keep them out of costly residential care homes shrank.
The only way she could afford help was to offer room and board to a series of live-in caregivers who she said abused alcohol and drugs and eventually subjected her to financial abuse. She vowed to never rely on live-in care again.
Now the 58-year-old Republican from the Inland Empire is worried Medicaid cuts being mulled by her party in Washington could force her into another vulnerable spot.
“If they reduce my budget, that doesn’t change the fact that I need 24-hour care,” said Ewing-Wilson, who has struggled with seizures and developmental disabilities her entire life. “If they cut it too much, people will die or they’ll lose their freedoms.”
Similar stories have already surfaced in GOP-held swing districts nationwide where activists have been applying political pressure to sway vulnerable House members from supporting $880 billion in cuts that health experts say would almost certainly hit safety net programs. But in California, which sends more Republicans to Congress than any state west of Texas, consumer groups and health industry giants are joining forces in a quieter campaign to lobby lawmakers in solidly red districts, some of which they say would be disproportionately affected if those cuts materialize.
Organizers are trying to highlight a thorny fact that faces many conservative members as they navigate a complex decision: The scale of spending cuts top GOP leaders are demanding is nearly impossible to achieve without slashing Medicaid funds to states, which are a lifeline for their largely poor, rural districts. In Rep. Doug LaMalfa’s northern Sierra district stretching to the Oregon border, for example, some 43% of residents are enrolled in Medi-Cal, while 48% of residents in Rep. Jay Obernolte’s district, centered on San Bernardino County, rely on Medi-Cal.
“The hospitals, the health plans — we don’t always get along with those folks,” said Dustin Corcoran, CEO of the powerful California Medical Association, which represents more than 55,000 doctors and encouraged its members to call their representatives. “On this, there’s not a lot of daylight. It will take strange bedfellows, for sure.”
The California Hospital Association has sent letters to Republican lawmakers and encouraged executives of its more than 400 member hospitals to reach out or provide tours to them. Consumer advocates and patient groups have protested outside members’ district offices and community health center CEOs have requested private meetings.
The House of Representatives in February approved a budget framework tasking the committee overseeing Medicaid to cut $880 billion over 10 years. While there are still no specific provisions cutting Medicaid, Medicare, or other safety net programs, health care analysts say the magnitude of the spending reductions means they’re inevitable. They could force millions of Californians off Medi-Cal (the state’s Medicaid program covers roughly 15 million people), reduce benefits for those still enrolled, and lower reimbursement rates for physicians at a time of acute provider shortages, said Kristof Stremikis, director of market analysis and insight for the California Health Care Foundation, a nonprofit that advocates on health care policy.
“What you’re talking about at the end of the day is reductions in funding that the states, including California, are in no position to make up,” Stremikis said. “You see that reflected in the different groups that have come together to talk about how important this program is.”
Even before Congress approved its controversial budget plan, Corcoran said, doctors and other industry representatives had been holding weekly calls for months to discuss how to protect Medicaid funding following Republicans’ substantial wins in November. Corcoran has also rallied physicians’ groups out of state, sending a joint letter to House leaders in February. The group has asked individual doctors to call or write their congressional representatives as well.
Many Republican lawmakers appear to be lying low while home after House leadership advised GOP members against holding in-person town halls, blaming Democratic activists for “hijacking” the events. A viral clip showed Obernolte getting booed down by constituents at a district event.
Meanwhile, LaMalfa said on the House floor in February that the spending resolution, which all nine California Republicans voted for, does not cut Medicaid, Medicare, or other social safety net programs.
“Any claim to the contrary is actually fearmongering, plain and simple, or I guess in my neighborhood it would be known as a lie,” he said.
Neither LaMalfa nor Obernolte responded to requests for comment.
Jo Campbell, who runs a federally qualified health center in LaMalfa’s district, said she has invited the lawmaker to join her and other local clinic executives to explain how the federal government can cut the $880 billion without touching funding crucial to health centers like hers.
“We all kind of live financially on a knife’s edge,” said Campbell, CEO of Hill Country Community Clinic, roughly half of whose patients rely on Medi-Cal. “It could mean the difference of whether or not we keep our doors open.”
Campbell hasn’t heard back from LaMalfa’s office.
Executives at Adventist Health, which has 23 hospitals across California, have met with Central Valley Republican Reps. Vince Fong and David Valadao and have requested a meeting with LaMalfa, with whom they worked closely after one of its hospitals burned in the 2018 Camp Fire.
“They’re all at different places,” said Adventist spokesperson Julia Drefke. “I think they understand what it means for their community. What that translates to in terms of their vote could be a different thing.”
In 2023, Medi-Cal made up more than 80% of patient revenue at Surprise Valley Community Hospital in LaMalfa’s district, for example, and 64% of patient revenue at Loma Linda University Children’s Hospital, in Obernolte’s district, came from Medi-Cal, according to a CHCF analysis of state data.
Sabrina Epstein, a policy analyst with Disability Rights California, said she’s encouraging local activists, no matter where they live, to engage with California’s congressional Republicans.
“It only takes a few votes to keep Medicaid going, to protect it in Congress,” she said. “We don’t know where those votes are going to come from.”
Republicans — swing district or not — will now have to weigh the popularity of Medicaid among their constituents with pressure from national Republicans who see a once-in-a-generation opportunity to shrink the size of government and have shown little mercy for party members who fall out of line. More than three-quarters of Americans have a favorable opinion of Medicaid, according to a January KFF poll.
Complicating that calculation is the recent revelation by Gov. Gavin Newsom’s administration that California’s Medi-Cal program is billions of dollars short and relying on a loan to cover the overrun. Republican state legislators have singled out California’s decision to cover low-income residents regardless of legal status, although other factors have also contributed.
“The majority party decided to add billions of dollars to the cost of Medi-Cal and it was so nonsensical,” said GOP Assembly member Joe Patterson. “That’s a self-inflicted wound.”
Jenny McLelland, whose 13-year-old son has a breathing disability that requires round-the-clock care, said cutting benefits for immigrants would end up costing taxpayers more, when they show up in emergency rooms with more complicated ailments.
“I don’t buy the argument that other people are any less deserving of care than my son,” said McLelland, who lives in Clovis, part of Fong’s district. For her son, Medi-Cal is “a matter of life and death,” she added.
She believes if Fong understood how vital Medi-Cal is to families, he would work to make the system better.
It remains to be seen whether targeting House Republicans will change minds when a final budget package is voted on. Two vulnerable members — Valadao and Young Kim, who represents a district east of Anaheim — have signaled they’ll oppose major cuts to Medicaid. Rep. Ken Calvert, whose Palm Desert district office was targeted by protesters during the spring recess, said in a statement that he favors work requirements and would not support Medicaid cuts for “mothers, children, disabled, and low-income Americans.”
In Valadao’s district, state data shows, two-thirds of residents rely on Medi-Cal, which is the single biggest payer for all five general acute care hospitals there. That includes Adventist Health Delano, which derives two-thirds of patient revenue from Medi-Cal, according to the CHCF analysis.
Most other GOP House members remain silent.
Ewing-Wilson voted for Obernolte, who won reelection by 20 percentage points and is in little danger of losing. She’s been trying for weeks to get a meeting with him. If he votes to cut Medicaid, she said, “I will be very disappointed in him, because I voted for him, expecting that he would care about all of his constituents.”
This article was produced by KFF Health News, which publishes California Healthline, an editorially independent service of the California Health Care Foundation.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).

by Admin
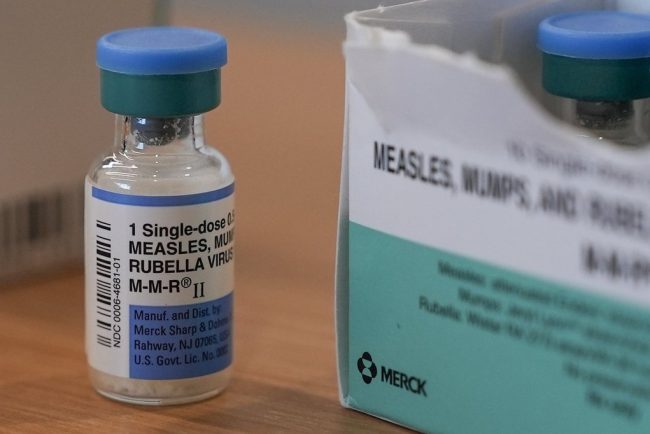
1.6K Ontario students suspended for old vaccination files amid measles outbreak
An Ontario public health unit has ordered the suspension of 1,624 elementary students for out-of-date vaccination records as a measles outbreak in the province continues.
MeaslesAn Ontario public health unit has ordered the suspension of 1,624 elementary students for out-of-date vaccination records as a measles outbreak in the province continues.

by Admin
Hit Hard by Opioid Crisis, Black Patients Further Hurt by Barriers to Care
CHARLOTTE, N.C. — Purple flags, representing the nearly 300 Mecklenburg County residents who died of opioid overdose in 2023, fluttered in the humid breeze last August in recognition of International Overdose Awareness Day on the city’s predominantly Black west side. As recently as five years […]
PharmaceuticalsCHARLOTTE, N.C. — Purple flags, representing the nearly 300 Mecklenburg County residents who died of opioid overdose in 2023, fluttered in the humid breeze last August in recognition of International Overdose Awareness Day on the city’s predominantly Black west side.
As recently as five years ago, the event might have attracted an overwhelmingly white crowd.
But the gathering on the last day of the month at the Valerie C. Woodard Community Resource Center drew large attendance from Black people eager to learn more about a crisis that now has them at the center.
In recent years, the rate of overdose deaths from opioids — originally dubbed “Hillbilly heroin” because of their almost exclusive misuse by white people — has grown significantly among Black people. This is largely due to the introduction of fentanyl, a synthetic opioid 50 to 100 times as powerful as morphine, which is often mixed into heroin and cocaine supplies and can be consumed unknowingly. In North Carolina, Black people died from an overdose at the rate of 38.5 per 100,000 residents in 2021 — more than double the rate in 2019, according to North Carolina Department of Health and Human Services data.
Terica Carter, founder of Hajee House Harm Reduction, a Charlotte-based nonprofit that co-organized the event with the county’s public health office, has been working to change that statistic. Seven years ago, she founded Hajee House after the overdose death of her 18-year-old son, Tahajee, who took an unprescribed dose of Percocet that he didn’t know was laced with fentanyl. Her nonprofit has since focused on addressing a critical issue in the fight against the opioid epidemic: that resources, treatment, and policy prescriptions have not followed the surge in addiction and overdoses among Black people.
“Nobody was acknowledging it, and I felt so alone,” Carter said. “That pushed me into not wanting anybody else to go through what I went through.”
Hajee House seeks to fill the gaps in resources and information about opioid overdose, substance use, and treatment. It also provides syringes, safe-use toolkits, the overdose reversal drug naloxone, fentanyl test strips, and recovery referral services — all in a familiar, neighborhood environment.
Despite efforts by groups like Hajee House, a lot of work remains in North Carolina. In 2019, for instance, white people accounted for 88% of those served by the opioid use prevention and treatment services funded by a $54 million grant from the federal Substance Abuse and Mental Health Services Administration, North Carolina Health News reported. Black people, meanwhile, made up about 24% of North Carolina’s population but only 7.5% of those served by the state assistance.
Nationally, Black people are half as likely as white people to be referred to or get treatment — even after a nonfatal overdose, according to the Centers for Disease Control and Prevention.
“If you are a Black person and have an opioid use disorder, you are likely to receive treatment five years later than if you’re a white person,” said Nora Volkow, director of the National Institute on Drug Abuse at the National Institutes of Health. “Five years can make the difference between being alive or not.”
According to the CDC, only 1 in 12 non-Hispanic Black people who died of an opioid overdose had been engaged in substance use treatment, while non-Hispanic white people had been treated at nearly twice the rate. Even those who seek care are less likely to complete the program and have poorer outcomes — which studies have linked to implicit bias and a lack of diversity and empathy for Black patients among treatment providers.

Daliah Heller, vice president of Drug Use Initiatives at Vital Strategies, a global health nonprofit, said she’s troubled by the lack of equal access to the full range of medications for opioid use disorder, which is considered the gold standard for care.
Those medications have the potential to reduce overdose risk by half and double a patient’s chances of entering long-term recovery. The FDA has approved three medications: buprenorphine and methadone, which are synthetic opioids that reduce cravings and withdrawal symptoms, and naltrexone, a post-detox monthly injectable that blocks the effects of opioids.
Black people are overwhelmingly treated with methadone. While methadone patients stay in treatment at higher rates compared with those prescribed buprenorphine, they face significant drawbacks, including difficulty finding a clinic, waitlists, and a requirement to visit the clinic every day to receive the medication under the supervision of a practitioner.
Meanwhile, buprenorphine can be prescribed in an office setting and filled at the pharmacy. A University of Michigan study found that white patients received buprenorphine three to four times as often as Black patients due to geographical availability and ability to pay.
“When buprenorphine came online in the early 2000s, we thought we could integrate that treatment alongside health care, and you wouldn’t need to go to a special program anymore,” Heller said. “That didn’t happen.”
Edwin Chapman, who runs an addiction clinic in Washington, D.C., said he must overcome many prescribing challenges to effectively treat his mostly Black patient population.
“The insurance companies in many states put more restrictions on patients in an urban setting, such as requiring prior authorization for addiction treatment,” Chapman said, speaking from his own experience working with patients. “The dosing standards were based on the white population and people who were addicted to pills. Our surviving Black population often needs a higher dose of buprenorphine.”

Heller said the lack of access to treatment is also driven by broader, systemic issues. She said many Black people fear that, by seeking social services, they might become ensnared in the criminal justice system and ultimately lose their employment, housing, or even custody of their children.
“Drug use occurs at the same levels across racial and ethnic groups, but Black Americans are more likely to be arrested and incarcerated on drug charges,” Heller said. “The more hyper-criminalized experience levied against Black communities interferes with access to care.”
All this is why there’s an increasing need for nonprofits like Hajee House that can provide information and a low-barrier access to services in the Black community, Carter said.
She credits the success of Hajee House to her personal connections and a keen understanding of the needs and cultural preferences of the Black community. When she holds overdose awareness events, for instance, she features cookouts, bouncy houses, and DJs to make them look more like block parties.
“We focus on making the events and outreach a comfortable, familiar environment for the Black community,” Carter said. “We’re Black, so we keep it Black.”
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).

by Admin
How Much Will That Surgery Cost? 🤷 Hospital Prices Remain Largely Unhelpful.
It’s a holy grail of health care: forcing the industry to reveal prices negotiated between health plans and hospitals — information that had long been treated as a trade secret. And among the flurry of executive orders President Donald Trump signed during his first five […]
Health CareIt’s a holy grail of health care: forcing the industry to reveal prices negotiated between health plans and hospitals — information that had long been treated as a trade secret. And among the flurry of executive orders President Donald Trump signed during his first five weeks back in office was a promise to “Make America Healthy Again” by giving patients accurate health care prices.
The goal is to force hospitals and health insurance companies to make it easier for consumers to compare the actual prices of medical procedures and prescription drugs. Trump gave his administration until the end of May to come up with a standard and a mechanism to make sure the health care industry complies.
But Trump’s 2025 order is also a symbol of how little progress the country has made since he issued a similar directive nearly six years ago. Consumers find it only partially useful, and the quality of the information is spotty.
A ‘Bold’ First Step That Fizzled
The 2019 order was “pretty bold,” said Gary Claxton, a senior vice president at KFF, a health information nonprofit that includes KFF Health News. “They basically went at the providers and the plans and said, ‘All this data you think is confidential we’re not going to make confidential anymore.’”
What followed was, to consumer advocacy groups, a disappointment. Hospitals and insurers posted on websites voluminous, complex, and confusing data about their prices. The information has been a challenge for even experts in health care pricing to navigate, let alone consumers. Some members of Congress filed legislation to put the force of law behind price transparency requirements; those bills died. And President Joe Biden’s administration was criticized for not more stringently enforcing the regulations, with one consumer advocacy group even buying a Super Bowl ad featuring the rapper Fat Joe alleging that “hospitals and insurers hide their prices.”
Trump’s new order, signed in February, said that hospitals and health plans “were not adequately held to account when their price transparency data was incomplete or not even posted at all.”
The Government Accountability Office reported in October that the Centers for Medicare & Medicaid Services didn’t know whether prices reported by the health care industry were correct or complete. But CMS, which regulates hospitals, now plans to “systematically monitor compliance” and help institutions understand the requirements, said Catherine Howden, an agency spokesperson.
Howden did not answer questions about whether CMS staffers overseeing price transparency compliance have been fired as part of the Trump administration’s wide-ranging effort to cut the federal workforce.
‘Zombie’ Rates and Other Inconsistencies
Meanwhile, independent researchers have found numerous problems with the quality of price data both hospitals and health insurers do share with consumers.
A recent report from the Peterson-KFF Health System Tracker found that data reported by four health insurers in New York City often included prices that they say they pay hospitals for services that those health providers don’t — or can’t — provide. These are called “ghost” or “zombie” rates. For example, the health plans reported dentists, optometrists, and audiologists receiving payments for knee replacements, gastrointestinal exams, and other procedures unrelated to their specialties.
In other cases, the data included different prices for the same service paid for by the same insurer at the same hospital. UnitedHealthcare, for example, reported paying New York-Presbyterian/Weill Cornell Medical Center three rates — $47,000, $64,000, and $70,000 — to treat a heart attack.
Or, the insurers reported paying the same price for vastly different services. Aetna, for example, said it paid exactly $6,292 to Mount Sinai Beth Israel hospital for the treatment of respiratory infections, heart attacks, cancers of the digestive tract, kidney and urinary tract infections, and psychosis.
Neither UnitedHealthcare nor Aetna addressed the discrepancies in the data. Cole Manbeck, a spokesperson for UnitedHealthcare, said the insurer has met price transparency requirements and urged members “to use our cost-estimator tools for exact costs based on their specific health plan.” Aetna spokesperson Shelly Bendit referred questions to AHIP, a lobbying and trade association for insurers.
Health insurers have “strongly supported” price transparency, said Chris Bond, a spokesperson for AHIP. The group will work with the Trump administration to provide transparency “in a way that is meaningful for the end user, while also promoting a competitive private market,” Bond said.
What’s a Consumer To Do?
Estimates and total prices aren’t very useful for consumers, who are mainly interested in what they’ll ultimately have to pay out-of-pocket, said David Cutler, a professor of applied economics at Harvard University. That can vary by health plan, depending on deductibles, copayments, and other fees.
“Most of the price transparency information doesn’t have that,” he said.
It also doesn’t give consumers information about the quality of care, Cutler added, which can lead to an old bias. “It’s kind of like wine when you go to the restaurant,” he said. “People assume that the more expensive wine is better.”
Cutler said he’s skeptical that price transparency will lower costs for patients. But he said it may offer insight to hospitals and health plans about what their competitors are charging and paying for services — knowledge that could inadvertently lead to price increases if hospitals that receive a lower rate than a competitor demand higher reimbursement from health plans.
Trump’s recent executive order notes that the top quarter of the most expensive health service prices have dropped by 6.3% a year since his 2019 order.
However, the same research referenced in the executive order showed that the bottom quarter of services got more expensive, at a rate of about 3.4% per year, according to the analysis by Turquoise Health, a health care price data firm that examined rates at more than 200 hospitals in the 10 largest U.S. markets.
Some patients say that with research and persistence, they’ve been able to make price transparency work for them.

Theresa Schmotzer, 50, of Goodyear, Arizona, said she used hospital price data to save nearly $3,000 on outpatient surgery to have a fibroid removed last year.
Schmotzer, who has health insurance, said the hospital first told her she would owe $3,700 for the procedure and wanted the payment upfront. But she was skeptical.
She said her health insurer was unable to quote a price for the procedure or specify how much she would owe. The morning of the surgery, Schmotzer said, she found a spreadsheet online at PatientRightsAdvocate.org that included different prices paid by insurers, including hers. The reported price for the procedure was closer to $700, she said.
Schmotzer said she took a printout of the spreadsheet to the hospital and presented it during preadmission. She paid her $300 deductible and told the hospital to bill her for the rest.
A few months later, she said, the bill arrived in the mail for the remaining $400, which she paid.
When people go for surgery and aren’t clear upfront what the cost will be, it stokes fear, she said. “Because they’re going in blind.”
Next Steps
Hospitals say they want to work with federal regulators and comply with reporting requirements, said Ariel Levin, director of coverage policy for the American Hospital Association, which represents about 5,000 institutions. Levin said consumers should be given the price of services and “a more comprehensive estimate” that represents an entire episode of care and the amount they’ll owe out-of-pocket, based on their health plan.
CMS has developed rules since Trump’s 2019 order to make price information reported by hospitals and health plans easier to understand, and the agency has fined more than a dozen hospitals for failing to comply.
Federal rules allow hospitals to report an estimate, a price range, or a historical rate for their services, while health plans can adjust prices based on factors like the severity of the case, the length of treatment, and a patient’s age.
KFF’s Claxton said that such flexibility doesn’t allow for “apples-to-apples comparisons” and that the data must be reliable before researchers can use it to better understand health care costs. “It doesn’t seem to be that yet,” he said.
Much remains to be done before price transparency lives up to expectations that it will increase competition and lower costs, said Katie Martin, chief executive of the Health Care Cost Institute, a nonprofit research group.
Price transparency alone is not a silver bullet, Martin said. It’s “a critical first step” for employers, lawmakers, regulators, and others to better understand how money flows through the health care system and how to make it more efficient, she said. “It’s not the whole thing.”
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).

by Admin
Rate of new measles cases in Ontario stable, says province’s top doctor
Ontario’s measles outbreak is likely to continue into the summer, the province’s chief medical officer of health said Friday, but he is hopeful it will not worsen.
MeaslesOntario’s measles outbreak is likely to continue into the summer, the province’s chief medical officer of health said Friday, but he is hopeful it will not worsen.

by Admin
Montana’s Small Pharmacies Behind Bill To Corral Pharmacy Benefit Managers
HELENA, Mont. — Montana’s small, independent pharmacies say they’re getting increasingly squeezed on reimbursements by pharmacy benefit managers — and are pushing an ambitious bill to rein in what they say are unfair practices by the powerful industry negotiators known as PBMs. “Who in their […]
Health CareHELENA, Mont. — Montana’s small, independent pharmacies say they’re getting increasingly squeezed on reimbursements by pharmacy benefit managers — and are pushing an ambitious bill to rein in what they say are unfair practices by the powerful industry negotiators known as PBMs.
“Who in their right mind would subject themselves to this sort of treatment in a business relationship?” said Mike Matovich, a part owner of eight small-town pharmacies in Montana. “It’s such a monopoly. We can be the best pharmacy in the world, and they can still put us out of business.”
The bill, which sailed through the Montana House 98-1 in early March and is now before the state Senate, would set a price floor that PBMs must pay pharmacies for each prescription. Currently, there is no mandated minimum rate in contracts with pharmacies, and independent drugstores said the rates are often below what they paid for the drugs.
The measure includes a half-dozen restrictions on other PBM practices the smaller pharmacies call anticompetitive.
Pharmacy benefit managers, employed by health insurers, are powerful intermediaries in the drug-pricing chain. They determine which drugs are covered by health plans, arrange rebates from drugmakers, and dictate payments that pharmacies receive when selling covered drugs.
The six largest PBMs manage more than 90% of the nation’s drug sales. Most are owned by or affiliated with health insurance giants like UnitedHealth Group, Cigna, Humana, and Aetna.
About 90 Montanan-owned pharmacies are not affiliated with national companies or PBMs, and 10 have closed in the past year, according to Josh Morris, who owns several small-town pharmacies in the state. Morris said his pharmacies lost $30,000 on underpaid drug claims last year and that they lose money on 90% of the brand-name drugs they dispense.

Representatives of independent Montana pharmacies say that without the changes provided by the legislation, more of their ranks will close, because they can’t make ends meet on drug reimbursement prices imposed by what they say are “take-it-or-leave-it” contracts from PBMs.
“We’re filling more prescriptions than ever before, but my employees haven’t had a raise in three years,” Morris said. “Our reimbursements are down 60% since 2019.”
PBMs are mounting a concerted effort in the Montana Senate to kill House Bill 740, arguing it could throw a huge wrench into drug pricing in Montana that would increase consumer costs.
“Not only is it going to cost people, it’s going to change fundamentally how prescription drugs are paid for in the state,” said Tonia Sorrell-Neal of the Pharmaceutical Care Management Association, a trade group representing PBMs. “It takes away the options for employers who are paying for these health plans” to keep drug prices low.
The bill restricts mail-order options for drugs, limits when PBMs can audit claims, and imposes excessive reimbursements, she said.
This battle between PBMs and independent pharmacies isn’t playing out just in Montana — it has roiled statehouses across the country, drawn the attention of Congress, and could end up before the U.S. Supreme Court.
Last summer, the federal House Oversight and Accountability Committee and the Federal Trade Commission issued highly critical reports saying PBMs use pricing tactics that keep drug costs high, help pad PBM profits, and harm independent pharmacies.
New federal regulations to crack down on PBMs had been included in a 2024 post-election budget bill before Congress but were stripped out at the last minute after a lobbying push by pharmacy benefit managers.
At least 20 states have passed laws regulating PBM payments to pharmacies and several other states, including California, are considering legislation this year.
Oklahoma passed one of the most expansive laws in 2019. But PBMs sued and won a federal court ruling that said the law does not apply to self-funded health plans, thus removing about two-thirds of the insured population from the law’s jurisdiction.
Oklahoma’s insurance commissioner last year asked the U.S. Supreme Court to overrule the decision, but the court hasn’t decided whether to take the case. Attorneys general from 31 states and the District of Columbia have asked the high court to rule in Oklahoma’s favor; Montana’s AG is not one of them.
In Montana, HB 740’s regulations would apply to PBMs managing self-funded plans, said the state insurance commissioner’s office, which so far supports the bill.
The key element of HB 740 is setting requirements on what PBMs must reimburse pharmacies for each prescription they fill, when that prescription is covered by a health plan using the PBM.
It says the reimbursement can be no less than 106% of the National Average Drug Acquisition Cost, or NADAC — which is determined by a survey of wholesale prices paid by pharmacies — plus a “dispensing fee” for each prescription.
The dispensing fee would be the same as what Montana’s Medicaid program pays pharmacies — $12 to $18 per prescription, depending on the size of the pharmacy. The state Medicaid program also pays the 106% minimum reimbursement.
Montana pharmacies say the dispensing fee covers their basic costs and enables them to make a profit on most sales. Under contracts with most PBMs, the pharmacies say they get no dispensing fee.
The bill also requires other changes in PBM business practices that pharmacies say benefit PBMs and make it harder for independent pharmacies to stay in business.
For example, HB 740 says PBMs cannot offer better prices to pharmacies that they own, cannot charge after-the-fact fees that lower reimbursement rates, cannot slow-walk approval of contracts, and cannot lower payments for drugs sold past a “sell-by” date imposed by the PBMs.
PBM and health plan lobbyists have attacked the bill for its breadth and detail, saying it’s so extensive that nobody truly knows how it may affect prescription-drug markets and prices in Montana.
“This bill has too much,” Bruce Spencer, an attorney for the Mountain Health Co-Op, told the House Business and Labor Committee at the bill’s first hearing in February. “It has unintended consequences that are severe in the financial world.”
Laura Shirtliff, a spokesperson for the state auditor’s office, said the bill’s provisions should be narrowed, to target assistance for smaller pharmacies.
PBM lobbyists are telling lawmakers to kill HB 740 and instead pass a bill to study the prescription-drug market in Montana, with an eye toward possible solutions to help rural pharmacies.
“I would say there are a lot of elements and factors that are impacting rural pharmacies’ business,” said Sorrell-Neal of the PBM trade group.
Supporters, however, said HB 740 needs to closely define exactly what’s happening in the field, between PBMs and pharmacies, so those practices can be regulated.
As for waiting two years for a study? Pharmacy owners say that’s too late, and that the time to fix the problem is now.
“The amount of damage that would be done in two years will never be able to be recovered from, in these communities,” Matovich said. “Ten years ago, we maybe lost money on five prescriptions a month. Now, it’s thousands of prescriptions a month.”
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).

by Admin
Check your measles vaccination, B.C. urges, as Ontario and Texas outbreaks grow
Health officials said they were concerned about the potential for measles to spread in B.C. as families return from overseas vacations in virus hotspots during spring break.
MeaslesHealth officials said they were concerned about the potential for measles to spread in B.C. as families return from overseas vacations in virus hotspots during spring break.

by Admin
Their Physical Therapy Coverage Ran Out Before They Could Walk Again
Mari Villar was slammed by a car that jumped the curb, breaking her legs and collapsing a lung. Amy Paulo was in pain from a femur surgery that wasn’t healing properly. Katie Kriegshauser suffered organ failure during pregnancy, weakening her so much that she couldn’t […]
Health CareMari Villar was slammed by a car that jumped the curb, breaking her legs and collapsing a lung. Amy Paulo was in pain from a femur surgery that wasn’t healing properly. Katie Kriegshauser suffered organ failure during pregnancy, weakening her so much that she couldn’t lift her baby daughter.
All went to physical therapy, but their health insurers stopped paying before any could walk without assistance. Paulo spent nearly $1,500 out of her own pocket for more sessions.
Millions of Americans rely on physical and occupational therapists to regain strength and motor skills after operations, diseases, and injuries. But recoveries are routinely stymied by a widespread constraint in health insurance policies: rigid caps on therapy sessions.
Insurers frequently limit such sessions to as few as 20 a year, a KFF Health News examination finds, even for people with severe damage such as spinal cord injuries and strokes, who may need months of treatment, multiple times a week. Patients can face a bind: Without therapy, they can’t return to work, but without working, they can’t afford the therapy.
Paulo said she pressed her insurer for more sessions, to no avail. “I said, ‘I’m in pain. I need the services. Is there anything I can do?’” she recalled. “They said, no, they can’t override the hard limit for the plan.”
A typical physical therapy session for a privately insured patient to improve daily functioning costs $192 on average, according to the Health Care Cost Institute. Most run from a half hour to an hour.
Insurers say annual visit limits help keep down costs, and therefore premiums, and are intended to prevent therapists from continuing treatment when patients are no longer improving. They say most injuries can be addressed in a dozen or fewer sessions and that people and employers who bought insurance could have purchased policies with better therapy benefits if it was a priority.
Atul Patel, a physiatrist in Overland Park, Kansas, and the treasurer of the American Academy of Physical Medicine and Rehabilitation, said insurers’ desire to prevent gratuitous therapy is understandable but has “gone too far.”
“Most patients get way less therapy than they would actually benefit from,” he said.
Hard caps on rehab endure in part because of an omission in the Affordable Care Act. While that law required insurers to cover rehab and barred them from setting spending restrictions on a patient’s medical care, it did not prohibit establishing a maximum number of therapy sessions a year.
More than 29,000 ACA health plans — nearly 4 in 5 — limit the annual number of physical therapy sessions, according to a KFF Health News analysis of plans sold last year to individuals and small businesses. Caps generally ranged from 20 to 60 visits; the most common was 20 a year.
Health plans provided by employers often have limits of 20 or 30 sessions as well, said Cori Uccello, senior health fellow at the American Academy of Actuaries.
“It’s the gross reality in America right now,” said Sam Porritt, chairman of the Falling Forward Foundation, a Kansas-based philanthropy that has paid for therapy for about 200 patients who exhausted their insurance over the past decade. “No one knows about this except people in the industry. You find out about it when tragedy hits.”
Even in plans with no caps, patients are not guaranteed unlimited treatment. Therapists say insurers repeatedly require prior authorization, demanding a new request every two or three visits. Insurers frequently deny additional sessions if they believe there hasn’t been improvement.
“We’re seeing a lot of arbitrary denials just to see if you’ll appeal,” said Gwen Simons, a lawyer in Scarborough, Maine, who represents therapy practices. “That’s the point where the therapist throws up their hands.”
‘Couldn’t Pick Her Up’
Katie Kriegshauser, a 37-year-old psychologist from Kansas City, Missouri, developed pregnancy complications that shut down her liver, pancreas, and kidneys in November 2023. After giving birth to her daughter, she spent more than three months in a hospital, undergoing multiple surgeries and losing more than 40 pounds so quickly that doctors suspected her nerves became damaged from compression. Her neurologist told her he doubted she would ever walk again.
Kriegshauser’s UnitedHealthcare insurance plan allowed 30 visits at Ability KC, a rehabilitation clinic in Kansas City. She burned through them in six weeks in 2024 because she needed both physical therapy, to regain her mobility, and occupational therapy, for daily tasks such as getting dressed.
“At that point I was starting to use the walker from being completely in the wheelchair,” Kriegshauser recalled. She said she wasn’t strong enough to change her daughter’s diaper. “I couldn’t pick her up out of her crib or put her down to sleep,” she said.
The Falling Forward Foundation paid for additional sessions that enabled her to walk independently and hold her daughter in her arms. “A huge amount of progress happened in that period after my insurance ran out,” she said.
In an unsigned statement, UnitedHealthcare said it covered the services that were included in Kriegshauser’s health plan. The company declined to permit an official to discuss its policies on the record because of security concerns.
A Shattered Teenager
Patients who need therapy near the start of a health plan’s year are more likely to run out of visits. Mari Villar was 15 and had been walking with high school friends to get a bite to eat in May 2023 when a car leaped over a curb and smashed into her before the driver sped away.
The accident broke both her legs, lacerated her liver, damaged her colon, severed an artery in her right leg, and collapsed her lung. She has undergone 11 operations, including emergency exploratory surgery to stop internal bleeding, four angioplasties, and the installation of screws and plates to hold her leg bones together.
Villar spent nearly a month in Shirley Ryan AbilityLab’s hospital in Chicago. She was discharged after her mother’s insurer, Blue Cross and Blue Shield of Illinois, denied her physician’s request for five more days, making her more reliant on outpatient therapy, according to records shared by her mother, Megan Bracamontes.

Villar began going to one of Shirley Ryan’s outpatient clinics, but by the end of 2023, she had used up the 30 physical therapy and 30 occupational therapy visits the Blue Cross plan allowed. Because the plan ran from July to June, she had no sessions left for the first half of 2024.
“I couldn’t do much,” Villar said. “I made lots of progress there, but I was still on crutches.”
Dave Van de Walle, a Blue Cross spokesperson, said in an email that the insurer does not comment on individual cases. Razia Hashmi, vice president for clinical affairs at the Blue Cross Blue Shield Association, said in a written statement that patients who have run out of sessions should “explore alternative treatment plans” including home exercises.
Villar received some extra sessions from the Falling Forward Foundation. While her plan year has reset, Villar is postponing most therapy sessions until after her next surgery so she will be less likely to run out again. Bracamontes said her daughter still can’t feel or move her right foot and needs three more operations: one to relieve nerve pain, and two to try to restore mobility in her foot by lengthening her Achilles tendon and transferring a tendon in her left leg into her right.
“Therapy caps are very unfair because everyone’s situation is different,” Villar said. “I really depend on my sessions to get me to a new normalcy. And not having that and going through all these procedures is scary to think about.”


Rationing Therapy
Most people who use all their sessions either stop going or pay out-of-pocket for extra therapy.
Amy Paulo, a 34-year-old Massachusetts woman recovering from two operations on her left leg, maxed out the 40 visits covered by Blue Cross Blue Shield of Massachusetts in 2024, so she spent $1,445 out-of-pocket for 17 therapy sessions.
Paulo needed physical therapy to recover from several surgeries to shorten her left leg to the length of her right leg — the difference a consequence of juvenile arthritis. Her recovery was prolonged, she said, because her femur didn’t heal properly after one of the operations, in which surgeons cut out the middle of her femur and put a rod in its place.
“I went ballistic on Blue Cross many, many times,” said Paulo, who works with developmentally delayed children.”
Amy McHugh, a Blue Cross spokesperson, declined to discuss Paulo’s case. In an email, she said most employers who hire Blue Cross to administer their health benefits choose plans with “our standard” 60-visit limit, which she said is more generous than most insurers offer, but some employers “choose to allow for more or fewer visits per year.”
Paulo said she expects to restrict her therapy sessions to once a week instead of the recommended twice a week because she’ll need more help after an upcoming operation on her leg.
“We had to plan to save my visits for this surgery, as ridiculous as it sounds,” she said.
Medicare Is More Generous
People with commercial insurance plans face more hurdles than those on Medicare, which sets dollar thresholds on therapy each year but allows therapists to continue providing services if they document medical necessity. This year the limits are $2,410 for physical and speech therapy and $2,410 for occupational therapy.
Private Medicare Advantage plans don’t have visit or dollar caps, but they often require prior authorization every few visits. The U.S. Senate Permanent Subcommittee on Investigations found last year that MA plans deny requests for physical and occupational therapy at hospitals and nursing homes at higher rates than they reject other medical services.
Therapists say many commercial plans require prior authorization and mete out approvals parsimoniously. Insurers often make therapists submit detailed notes, sometimes for each session, documenting patients’ treatment plans, goals, and test results showing how well they perform each exercise.
“It’s a battle of getting visits,” said Jackee Ndwaru, an occupational therapist in Jacksonville, Florida. “If you can’t show progress they’re not going to approve.”
An Insurer Overruled
Marjorie Haney’s insurance plan covered 20 therapy sessions a year, but Anthem Blue Cross Blue Shield approved only a few visits at a time for the rotator cuff she tore in a bike accident in Maine. After 13 visits in 2021, Anthem refused to approve more, writing that her medical records “do not show you made progress with specific daily tasks,” according to the denial letter.
Haney, a physical therapist herself, said the decision made no sense because at that stage of her recovery, the therapy was focused on preventing her shoulder from freezing up and gradually expanding its range of motion.
“I went through those visits like they were water,” Haney, now 57, said. “My range was getting better, but functionally I couldn’t use my arm to lift things.”
Haney appealed to Maine’s insurance bureau for an independent review. In its report overturning Anthem’s decision, the bureau’s physician consultant, William Barreto, concluded that Haney had made “substantial improvement” — she no longer needed a shoulder sling and was able to return to work with restrictions. Barreto also noted that nothing in Anthem’s policy required progress with specific daily tasks, which was the basis for Anthem’s refusal.
“Given the member’s substantial restriction in active range of motion and inability to begin strengthening exercises, there is remaining deficit that requires the skills and training of a qualified physical therapist,” the report said.
Anthem said it requires repeated assessments before authorizing additional visits “to ensure the member is receiving the right care for the right period of time based on his or her care needs.” In the statement provided by Stephanie DuBois, an Anthem spokesperson, the insurer said this process “also helps prevent members from using up all their covered treatment benefits too quickly, especially if they don’t end up needing the maximum number of therapy visits.”
In 2023, Maine passed a law banning prior authorization for the first 12 rehab visits, making it one of the few states to curb insurer limitations on physical therapy. The law doesn’t protect residents with plans based in other states or plans from a Maine employer who self-insures.
Haney said after she won her appeal, she spaced out the sessions her plan permitted by going once weekly. “I got another month,” she said, “and I stretched it out to six weeks.”
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).
by Admin
He Had Short-Term Health Insurance. His Colonoscopy Bill: $7,000.
Tim Winard knew he needed to buy health insurance when he left his management job in manufacturing to launch his own business. It was the first time he had shopped around for coverage, searching for a plan that would cover him and his wife, who […]
Health CareTim Winard knew he needed to buy health insurance when he left his management job in manufacturing to launch his own business.
It was the first time he had shopped around for coverage, searching for a plan that would cover him and his wife, who was also between jobs at the time.
“We were so nervous about not being on a company-provided plan,” Winard said.
After speaking with an insurance agent, he decided against enrolling in an Affordable Care Act plan because he was concerned about the potential cost. Instead, he chose a short-term policy, good for six months.
Six months later, Winard was still working on starting his business, so he signed up for another short-term policy with a different insurer that cost about $500 a month.
When he needed a colonoscopy, Winard, 57, called his insurance company. He said a representative told him to go to any facility he wanted for the procedure.
Early last year, he had the colonoscopy at a hospital in Elmhurst, Illinois, not far from his home in Addison.
The procedure went well, and Winard went home right afterward.
Then the bill came.
The Medical Procedure
Periodic colon cancer screening is recommended for people at average risk starting at age 45 and continuing until age 75, according to the U.S. Preventive Services Task Force. In addition to those for preventive purposes, doctors may order colonoscopies to diagnose existing concerns, as was the case for Winard.
There are several ways to screen, including noninvasive stool tests. A colonoscopy allows clinicians to examine and remove any polyps, which are then tested to see whether they are precancerous or malignant.
The Final Bill
$10,723.19, including $1,436 for the anesthesia and $1,039 for the recovery room. After an insurance discount, his plan paid $817.47. Winard was left owing $7,226.71.
The Billing Problem: A Short-Term Plan, With Coverage Caps and Gaps
Short-term, limited-duration insurance policies do not have to follow rules established under the ACA because they are intended to be only temporary coverage.
As Winard experienced, benefits within the plans can vary, with some setting specific dollar caps on certain types of medical care — sometimes far below what it costs. What’s covered can be hard to parse, and the insurer generally gets the last word on interpreting its rules.
While some short-term policies look like comprehensive major medical policies, all come with significant caveats. Most have limits that people accustomed to work-based or comprehensive ACA plans may find surprising.
All short-term insurance carriers, for example, screen applicants for health conditions and can reject them because of health problems or exclude those conditions. Many do not include drug coverage or maternity care.
The fact that short-term plans can cover fewer services, conditions, and patients is why they are generally less expensive than an unsubsidized ACA plan.

“The general trade-off is lower premiums versus what the plans actually cover,” said Cynthia Cox, vice president and director of the program on the ACA at KFF, a health information nonprofit that includes KFF Health News. “But the reason short-term plans are priced lower than a more comprehensive ACA plan is that they can deny people with preexisting conditions and don’t have to cover a lot of essential health benefits.”
Stunned that he owed more than $7,000 for his colonoscopy, Winard contacted his insurance company, Companion Life Insurance of Columbia, South Carolina.
An insurance representative told him in an email that it classified the procedure and all its costs, including the anesthesia, under his policy’s “outpatient surgery facility” benefit.
That benefit, the email said, capped insurance payment “within that facility” to a maximum of $1,000 per day.
That definition surprised Winard, who said he read his policy to mean that there was a cap on what could be charged for the facility itself — not for all the care he received there.
“I interpreted it to be a facility like a recovery room or surgery room,” he said. “They defined it to include any services at an outpatient facility.”
His plan says it covers colon cancer screening at 80% after patients meet their deductible. It also covers 80% of the cost of drugs provided in an outpatient setting.
Winard, who had met his deductible, said he expected he would pay only 20% toward the cost of his colonoscopy. But he also wondered why the screening, performed at Endeavor Health Elmhurst Hospital, was categorized by the insurer as a procedure at an “outpatient” facility.
According to the email Winard received from his insurer, his policy’s $1,000-a-day limit applies to “treatment or services in a state-approved freestanding ambulatory surgery center that is not part of a hospital, or a hospital outpatient surgery facility.”
Elmhurst Health spokesperson Allie Burke said that the hospital has an attached building where same-day outpatient procedures like colonoscopies are performed.
Short-term plans have been sold for decades. But in recent years, they’ve become a political football.
Out of concern that people would choose them over more comprehensive ACA insurance, President Barack Obama’s administration limited short-term plans’ terms to three months. Those rules were lifted in President Donald Trump’s first term, allowing the plans to again be sold as 364-day policies.
President Joe Biden, calling such plans “junk insurance,” restricted the policies to four months — a change that took effect one month after Winard’s procedure. Trump is expected to reverse Biden’s reversal and again make them available for longer durations.
The Resolution
In December, Winard hired an advocate, Linda Michelson, to help him parse his bill. They wrote to the hospital, offering to pay $4,000 if it would settle the entire bill — an amount Michelson said is about four times what Medicare would pay for a colonoscopy. Winard said the hospital declined the offer.
Spencer Walrath, another Elmhurst spokesperson, wrote in an email to KFF Health News that the hospital’s prices “reflect the value of the services we deliver.”
Companion Life did not respond to requests for comment. Scott Wood, who identified himself as a program manager and co-founder of Pivot Health, which markets Companion Life and other insurance plans, said in an interview that there was room for interpretation in the billing and that he had asked Companion Life to take another look.
Shortly after Wood’s comment to KFF Health News, Winard said he was contacted by his insurer. A representative told him that, upon reconsideration, the bill had been adjusted — although he was given no specific explanation as to why.
His new bill showed he owed only $770.

The Takeaway
Short-term plans can be appealing for some people because of the relatively low cost of their premiums, but consumers should read all the plan documents carefully before enrolling. Understand that the plans often won’t cover a full range of benefits, and check to see which services are covered and which are excluded. Check whether a policy includes per-day or per-policy-period dollar caps on coverage or other payout limits.
The federal government offers subsidies based on household income for ACA plans, which can make them comparable in cost to cheaper, short-term plans — but with a wider range of benefits.
In hindsight, Winard said he had not understood the difference between ACA policies and short-term plans.
His advice? Don’t rely solely on marketing materials, and always get a cost estimate, preferably in writing, before a nonemergency procedure like a colonoscopy.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).
by Admin
SHA issues measles exposure warning in Saskatoon and North Battleford
The Saskatchewan Health Authority (SHA) is warning the public about potential measles exposure in Saskatoon and North Battleford after the third confirmed case of measles.
MeaslesThe Saskatchewan Health Authority (SHA) is warning the public about potential measles exposure in Saskatoon and North Battleford after the third confirmed case of measles.