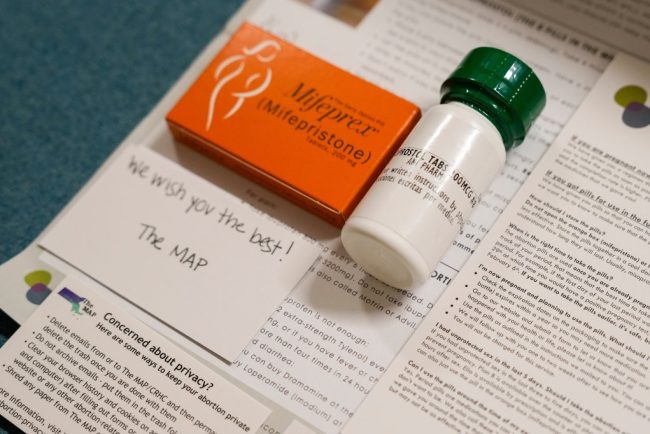
Despite Historic Indictment, Doctors Will Keep Mailing Abortion Pills Across State Lines
When the news broke on Jan. 31 that a New York physician had been indicted for shipping abortion medications to a woman in Louisiana, it stoked fear across the network of doctors and medical clinics who engage in similar work. “It’s scary. It’s frustrating,” said […]
Pharmaceuticals
At Social Security, These Are the Days of the Living Dead
Rennie Glasgow, who has served 15 years at the Social Security Administration, is seeing something new on the job: dead people. They’re not really dead, of course. In four instances over the past few weeks, he told KFF Health News, his Schenectady, New York, office […]
Health Care
HIV Testing and Outreach Falter as Trump Funding Cuts Sweep the South
JACKSON, Miss. — Storm clouds hung low above a community center in Jackson, where pastor Andre Devine invited people inside for lunch. Hoagies with smoked turkey and ham drew the crowd, but several people lingered for free preventive health care: tests for HIV and other […]
Health Care

Covid Worsened Shortages of Doctors and Nurses. Five Years On, Rural Hospitals Still Struggle.
Even by rural hospital standards, Keokuk County Hospital and Clinics in southeastern Iowa is small. The 14-bed hospital, in Sigourney, doesn’t do surgeries or deliver babies. The small 24-hour emergency room is overseen by two full-time doctors. CEO Matt Ives wants to hire a third […]
Rural HealthEven by rural hospital standards, Keokuk County Hospital and Clinics in southeastern Iowa is small.
The 14-bed hospital, in Sigourney, doesn’t do surgeries or deliver babies. The small 24-hour emergency room is overseen by two full-time doctors.
CEO Matt Ives wants to hire a third doctor, but he said finding physicians for a rural area has been challenging since the covid-19 pandemic. He said several physicians at his hospital have retired since the start of the pandemic, and others have decided to stop practicing certain types of care, particularly emergency care.
Another rural hospital is down the road, about a 40-minute drive east. Washington County Hospital and Clinics has 22 beds and is experiencing similar staffing struggles. “Over the course of the last few years, we’ve had not only the pandemic, but we’ve had kind of an aging physician workforce that has been retiring,” said Todd Patterson, CEO.
The pandemic was difficult for health workers. Many endured long hours, and the stresses on the nation’s health care system prompted more workers than usual to quit or retire.
“There’s a chunk of workers that were lost and won’t come back,” said Joanne Spetz, who directs the Institute for Health Policy Studies at the University of California-San Francisco. “For a lot of the clinicians that decided and were able to stick it out and work through the pandemic, they have burned out,” Spetz said.
Five years after the World Health Organization declared covid a global pandemic and the first Trump administration announced a national emergency, the United States faces a crucial shortage of medical providers, below the projected need for an aging population.
That could have lasting effects on care, particularly in states like Iowa with significant rural populations. Experts say the problem has been building for a while, but the effects of the pandemic accelerated the shortages by pushing many doctors over the edge into early retirement or other fields.
“Some of them made it through covid like ‘Let’s get us through this public health crisis,’ and then they came out of it saying, ‘OK, and now? Now I’m exhausted,’” said Christina Taylor, president of the Iowa Medical Society.
“Iowa is absolutely in the middle of a physician shortage,” Taylor said. “It’s a true crisis for us. We’re actually 44th in the country in terms of patient-to-physician ratio.”
A 2022 survey by the Centers for Disease Control and Prevention found a significant jump in health workers who reported feeling burned out and wanting a new job, compared with 2018. The number of people in health care has grown since the start of the pandemic, said Janette Dill, an associate professor at the University of Minnesota’s School of Public Health, but the growth has not happened fast enough.
“We have an aging population. We have a lot of needs,” she said.
The Association of American Medical Colleges projected last year that the U.S. faces a shortage of up to 86,000 physicians by 2036 — if lawmakers don’t invest more money in training doctors.
These shortages could push more people to seek care in ERs when they can’t see a local doctor, said Michael Dill, director of workforce studies at the AAMC.
“We’re already at a point where tens of millions of Americans every year can’t get medical care when they need it,” said Dill (no relation to Janette Dill). “If the shortage is sustained or gets even worse, then that problem gets worse too, and it disproportionately negatively impacts the most vulnerable amongst us.”
Iowa lawmakers made addressing the shortage a priority in the current legislative session. They introduced bills aimed at increasing medical student loan forgiveness and requesting federal help to add residency training slots for medical students in the state.
Last year, Gov. Kim Reynolds signed a bill into law that drops the residency requirement for some doctors who trained abroad to get a medical license. Lawmakers in at least eight other states have approved similar changes.
Patterson, of the Washington County hospital, appreciates that Iowa lawmakers are trying to increase the pipeline of doctors into Iowa but said it doesn’t address immediate shortages.
“You have a high school student who’s graduating right now; they’re probably nine to 11 years away from entering the workforce as a practicing physician. So it’s a long-term kind of problem,” he said.
For nurses, workforce experts say, the projected national outlook isn’t as dire as in recent years.
“Nursing education is back up. Nursing employment rates are back up. I think, for that workforce, we’ve largely nationally recovered from all the dislocations that occurred,” said Spetz, of the Institute for Health Policy Studies.
But getting nurses to move to the places that need them, like rural communities, will be difficult, she said.
Some rural hospitals in Iowa say an even bigger challenge right now is finding nurses to hire.

Some of that can be traced to the pandemic, said Sara Bruns, nurse manager at Keokuk County Hospital and Clinics. She recalled that some covid patients in critical condition died when they couldn’t be transferred to larger hospitals with more advanced intensive care unit equipment, because those hospitals didn’t have the staff to take on more patients.
“We had to make the horrible decision of ‘You’re probably not going to make it,’” Bruns recalled, saying many patients were then listed as DNR, for “do not resuscitate.”
“That took a big toll on a lot of nurses,” she said.
Another problem is persuading the area’s young nurses to stay, when they would rather live and work in more urban areas, Bruns said.
Her hospital still relies on contracts with travel nurses to fill some night shifts. That’s something the hospital never had to do before the pandemic, Bruns said. Travel nurses are more expensive, adding stress to a small hospital’s budget.
“I think some people just completely got out of nursing,” Bruns said. The pandemic took a special toll “because of the hours that they had to work, the conditions that they had to work.”
Policymakers and health care organizations can’t focus only on recruiting workers, according to Janette Dill at the University of Minnesota. “You also have to retain workers,” she said. “You can’t just recruit new people and then have them be miserable.”
Dill said workers report feeling that patients have been more disrespectful and challenging since the pandemic, and sometimes workers feel unsafe at work. “By ‘unsafe’ I mean physically unsafe. I think that is a very stressful part of the job,” she said.
Research has shown health workers reporting higher levels of burnout and poor mental health since the pandemic — though the risks decreased if workers felt supported by their managers.
Gail Grimes, an intensive care nurse in Des Moines, felt more supported by her employer during the worst parts of the pandemic than she does now, she said. Some hospitals offered pay bumps and more scheduling flexibility to keep nurses on staff.
“We were getting better bonus pay,” Grimes recalled. “We were getting these specialized contracts we could fulfill that were often more worth our time to be able to come in, to miss our families and be there.”
Grimes said she’s seen nurses leave Iowa for neighboring states with better average pay. This creates shortages that she believes affect the care she gives her own patients.
“A nurse taking care of five patients will always be able to provide better care than a nurse taking care of 10 patients,” she said.
She thinks many hospitals have simply accepted staff burnout as a fact, rather than try to prevent it.
“It really is significantly impactful to your mental health when you come home every day and you feel guilty about the things you have not been able to provide to people,” she said.
This article is from a partnership that includes IPR, NPR, and KFF Health News.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).

Watch: Why Insurance Companies Are Denying Coverage for Prosthetic Limbs
PBS News Weekend’s Ali Rogin spoke with KFF Health News contributor Michelle Andrews about what some people with missing limbs consider a disparity in health insurance coverage: Though a knee replacement likely would be covered, a prosthetic knee isn’t always. A prosthetic device can be […]
Health CarePBS News Weekend’s Ali Rogin spoke with KFF Health News contributor Michelle Andrews about what some people with missing limbs consider a disparity in health insurance coverage: Though a knee replacement likely would be covered, a prosthetic knee isn’t always. A prosthetic device can be subject to cost caps and an amputee may be required to prove medical necessity for coverage. Andrews recently explored these issues in her article “Health Insurers Limit Coverage of Prosthetic Limbs, Questioning Their Medical Necessity.”
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).

More than 100 new measles cases reported in Ontario as total reaches 925
Measles has spread to 109 more people in Ontario over the last week, bringing the province’s total cases to 925 since an outbreak began in October.
MeaslesMeasles has spread to 109 more people in Ontario over the last week, bringing the province’s total cases to 925 since an outbreak began in October.

Beyond Ivy League, RFK Jr.’s NIH Slashed Science Funding Across States That Backed Trump
The National Institutes of Health’s sweeping cuts of grants that fund scientific research are inflicting pain almost universally across the U.S., including in most states that backed President Donald Trump in the 2024 election. A KFF Health News analysis underscores that the terminations are sparing […]
Rural HealthThe National Institutes of Health’s sweeping cuts of grants that fund scientific research are inflicting pain almost universally across the U.S., including in most states that backed President Donald Trump in the 2024 election.
A KFF Health News analysis underscores that the terminations are sparing no part of the country, politically or geographically. About 40% of organizations whose grants the NIH cut in its first month of slashing, which started Feb. 28, are in states Trump won in November.
The Trump administration has singled out Ivy League universities including Columbia and Harvard for broad federal funding cuts. But the spending reductions at the NIH, the nation’s foremost source of funding for biomedical research, go much further: Of about 220 organizations that had grants terminated, at least 94 were public universities, including flagship state schools in places such as Florida, Georgia, Ohio, Nebraska, and Texas.
The Trump administration has canceled hundreds of grants supporting research on topics such as vaccination; diversity, equity, and inclusion; and the health of LGBTQ+ populations. Some of the terminations are a result of Trump’s executive orders to abandon federal work on diversity and equity issues. Others followed the Senate confirmation of anti-vaccine activist Robert F. Kennedy Jr. to lead the Department of Health and Human Services, which oversees the NIH. Many mirror the ambitions laid out in Project 2025’s “Mandate for Leadership,” the conservative playbook for Trump’s second term.
Affected researchers say Trump administration officials are taking a cudgel to efforts to improve the lives of people who often experience worse health outcomes — ignoring a scientific reality that diseases and other conditions do not affect all Americans equally.
KFF Health News found that the NIH terminated about 780 grants or parts of grants between Feb. 28 and March 28, based on documents published by the Department of Health and Human Services and a list maintained by academic researchers. Some grants were canceled in full, while in other cases, only supplements — extra funding related to the main grant, usually for a shorter-term, related project — were terminated.
Among U.S. recipients, 96 of the institutions that lost grants in the first month are in politically conservative states including Florida, Ohio, and Indiana, where Republicans control the state government or voters reliably support the GOP in presidential campaigns, or in purple states such as North Carolina, Michigan, and Pennsylvania that were presidential battleground states. An additional 124 institutions are in blue states.
Sybil Hosek, a research professor at the University of Illinois-Chicago, helps run a network that focuses on improving care for people 13 to 24 years old who are living with or at risk for HIV. The NIH awarded Florida State University $73 million to lead the HIV project.
“We never thought they would destroy an entire network dedicated to young Americans,” said Hosek, one of the principal investigators of the Adolescent Medicine Trials Network for HIV/AIDS Interventions. The termination “doesn’t make sense to us.”
NIH official Michelle Bulls is director of the Office of Policy for Extramural Research Administration, which oversees grants policy and compliance across NIH institutes. In terminating the grant March 21, Bulls wrote that research “based primarily on artificial and nonscientific categories, including amorphous equity objectives, are antithetical to the scientific inquiry, do nothing to expand our knowledge of living systems, provide low returns on investment, and ultimately do not enhance health, lengthen life, or reduce illness.”
Adolescents and young adults ages 13 to 24 accounted for 1 in 5 new HIV infections in the U.S. in 2022, according to the Centers for Disease Control and Prevention.
“It’s science in its highest form,” said Lisa Hightow-Weidman, a professor at Florida State University who co-leads the network. “I don’t think we can make America healthy again if we leave youth behind.”
HHS spokesperson Emily Hilliard said in an emailed statement that “NIH is taking action to terminate research funding that is not aligned with NIH and HHS priorities.” The NIH and the White House didn’t respond to requests for comment.
“As we begin to Make America Healthy Again, it’s important to prioritize research that directly affects the health of Americans. We will leave no stone unturned in identifying the root causes of the chronic disease epidemic as part of our mission to Make America Healthy Again,” Hilliard said.
Harm to HIV, Vaccine Studies
The NIH, with its nearly $48 billion annual budget, is the largest public funder of biomedical research in the world, awarding nearly 59,000 grants in the 2023 fiscal year. The Trump administration has upended funding for projects that were already underway, stymied money for new applications, and sought to reduce how much recipients can spend on overhead expenses.
Those changes — plus the firing of 1,200 agency employees as part of mass layoffs across the government — are alarming scientists and NIH workers, who warn that they will undermine progress in combating diseases and other threats to the nation’s public health. On April 2, the American Public Health Association, Ibis Reproductive Health, and affected researchers, among others, filed a lawsuit in federal court against the NIH and HHS to halt the grant cancellations.
Two National Cancer Institute employees, who were granted anonymity because they were not authorized to speak to the press and feared retaliation, said its staff receives batches of grants to terminate almost daily. On Feb. 27, the cancer institute had more than 10,800 active projects, the highest share of the NIH’s roughly two dozen institutes and centers, according to the NIH’s website. At least 47 grants that NCI awarded were terminated in the first month.
Kennedy has said the NIH should take a years-long pause from funding infectious disease research. In November 2023, he told an anti-vaccine group, “I’m gonna say to NIH scientists, ‘God bless you all. Thank you for public service. We’re going to give infectious disease a break for about eight years,’” according to NBC News.
For years, Kennedy has peddled falsehoods about vaccines — including that “no vaccine” is “safe and effective,” and that “there are other studies out there” showing a connection between vaccines and autism, a link that has repeatedly been debunked — and claimed falsely that HIV is not the only cause of AIDS.
KFF Health News found that grants in blue states were disproportionately affected, making up roughly two-thirds of terminated grants, many of them at Columbia University. The university had more grants terminated than all organizations in politically red states combined. On April 4, Democratic attorneys general in 16 states sued HHS and the NIH to block the agency from canceling funds.
Researchers whose funding was stripped said they stopped clinical trials and other work on improving care for people with HIV, reducing vaping and smoking rates among LGBTQ+ teens and young adults, and increasing vaccination rates for young children. NIH grants routinely span several years.
For example, Hosek said that when the youth HIV/AIDS network’s funding was terminated, she and her colleagues were preparing to launch a clinical trial examining whether a particular antibiotic that is effective for men to prevent sexually transmitted infections would also work for women.
“This is a critically important health initiative focused on young women in the United States,” she said. “Without that study, women don’t have access to something that men have.”
Other scientists said they were testing how to improve health outcomes among newborns in rural areas with genetic abnormalities, or researching how to improve flu vaccination rates among Black children, who are more likely to be hospitalized and die from the virus than non-Hispanic white children.
“It’s important for people to know that — if, you know, they are wondering if this is just a waste of time and money. No, no. It was a beautiful and rare thing that we did,” said Joshua Williams, a pediatric primary care doctor at Denver Health in Colorado who was researching whether sharing stories about harm experienced due to vaccine-preventable diseases — from missed birthdays to hospitalizations and job loss — might inspire caregivers to get their children vaccinated against the flu.
He and his colleagues had recruited 200 families, assembled a community advisory board to understand which vaccinations were top priorities, created short videos with people who had experienced vaccine-preventable illness, and texted those videos to half of the caregivers participating in the study.
They were just about to crack open the medical records and see if it had worked: Were the group who received the videos more likely to follow through on vaccinations for their children? That’s when he got the notice from the NIH.
“It is the policy of NIH not to prioritize research activities that focuses gaining scientific knowledge on why individuals are hesitant to be vaccinated and/or explore ways to improve vaccine interest and commitment,” the notice read.
Williams said the work was already having an impact as other institutions were using the idea to start projects related to cancer and dialysis.
A Hit to Rural Health
Congress previously tried to ensure that NIH grants also went to states that historically have had less success obtaining biomedical research funding from the government. Now those places aren’t immune to the NIH’s terminations.
Sophia Newcomer, an associate professor of public health at the University of Montana, said she had 18 months of work left on a study examining undervaccination among infants, which means they were late in receiving recommended childhood vaccines or didn’t receive the vaccines at all. Newcomer had been analyzing 10 years of CDC data about children’s vaccinations and had already found that most U.S. infants from 0 to 19 months old were not adequately vaccinated.
Her grant was terminated March 10, with the NIH letter stating the project “no longer effectuates agency priorities,” a phrase replicated in other termination letters KFF Health News has reviewed.
“States like Montana don’t get a lot of funding for health research, and health researchers in rural areas of the country are working on solutions to improve rural health care,” Newcomer said. “And so cuts like this really have an impact on the work we’re able to do.”
Montana is one of 23 states, along with Puerto Rico, that are eligible for the NIH’s Institutional Development Award program, meant to bolster NIH funding in states that historically have received less investment. Congress established the program in 1993.
The NIH’s grant terminations hit institutions in 15 of those states, more than half that qualify, plus Puerto Rico.
Researchers Can’t ‘Just Do It Again Later’
The NIH’s research funds are deeply entrenched in the U.S. health care system and academia. Rarely does an awarded grant stay within the four walls of a university that received it. One grant’s money is divvied up among other universities, hospitals, community nonprofits, and other government agencies, researchers said.
Erin Kahle, an infectious disease epidemiologist at the University of Michigan, said she was working with Emory University in Georgia and the CDC as part of her study. She was researching the impact of intimate partner violence on HIV treatment among men living with the virus. “They are relying on our funds, too,” she said.
Kahle said her top priority was to ethically and safely wind down her nationwide study, which included 418 people, half of whom were still participating when her grant was terminated in late March. Kahle said that includes providing resources to participants for whom sharing experiences of intimate partner violence may cause trauma or mental health distress.
Rachel Hess, the co-director of the Clinical & Translational Science Institute at the University of Utah, said the University of Nevada-Reno and Intermountain Health, one of the largest hospital systems in the West, had received funds from a $38 million grant that was awarded to the University of Utah and was terminated March 12.
The institute, which aims to make scientific research more efficient to speed up the availability of treatments for patients, supported over 5,000 projects last year, including 550 clinical trials with 7,000 participants. Hess said that, for example, the institute was helping design a multisite study involving people who have had heart attacks to figure out the ideal mix of medications “to keep them alive” before they get to the hospital, a challenge that’s more acute in rural communities.
After pushback from the university — the institute’s projects included work to reduce health care disparities between rural and urban areas — the NIH restored its grant March 29.
Among the people the Utah center thanked in its announcement about the reversal were the state’s congressional delegation, which consists entirely of Republican lawmakers. “We are grateful to University of Utah leadership, the University of Utah Board of Trustees, our legislative delegation, and the Utah community for their support,” it said.
Hilliard, of HHS, said that “some grants have been reinstated following the appeals process, and the agency will continue to carry out the remaining appeals as planned to determine their alignment.” She declined to say how many had been reinstated, or why the University of Utah grant was among them.
Other researchers haven’t had the same luck. Kahle, in Michigan, said projects like hers can take a dozen years from start to finish — applying for and receiving NIH funds, conducting the research, and completing follow-up work.
“Even if there are changes in the next administration, we’re looking at at least a decade of setting back the research,” Kahle said. “It’s not as easy as like, ‘OK, we’ll just do it again later.’ It doesn’t really work that way.”
Methodology
KFF Health News analyzed National Institutes of Health grant data to determine the states and organizations most affected by the Trump administration’s cuts.
We tallied the number of terminated NIH grants using two sources: a Department of Health and Human Services list of terminated grants published April 4; and a crowdsourced list maintained by Noam Ross of rOpenSci and Scott Delaney of the Harvard T.H. Chan School of Public Health, as of April 8. We focused on the first month of terminations: from Feb. 28 to March 28. We found that 780 awards were terminated in total, with 770 of them going to recipients based in U.S. states and two to recipients in Puerto Rico.
The analysis does not account for potential grant reinstatements, which we know happened in at least one instance.
Additional information on the recipients, such as location and business type, came from the USAspending.gov Award Data Archive.
There were 222 U.S. recipients in total. At least 94 of them were public higher education institutions. Forty-one percent of organizations that had NIH grants cut in the first month were in states that President Donald Trump won in the 2024 election.
Some recipients, including the University of Texas MD Anderson Cancer Center and Vanderbilt University Medical Center, are medical facilities associated with higher education institutions. We classified these as hospitals/medical centers.
We also wanted to see whether the grant cuts affected states across the political spectrum. We generally classified states as blue if Democrats control the state government or Democratic candidates won them in the last three presidential elections, and red if they followed this pattern but for Republicans. Purple states are generally presidential battleground states or those where voters regularly split their support between the two parties: Arizona, Michigan, Nevada, New Hampshire, North Carolina, Pennsylvania, Virginia, and Wisconsin. The result was 25 red states, 17 blue states, and eight purple states. The District of Columbia was also blue.
We found that, of affected U.S. institutions, 96 were in red or purple states and 124 were in blue states.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).

Quebec on verge of declaring measles outbreak over after no new cases in weeks
Quebec’s ministry of health says it’s on the verge of declaring its measles outbreak over, just as cases reach new heights in other parts of the country.
MeaslesQuebec’s ministry of health says it’s on the verge of declaring its measles outbreak over, just as cases reach new heights in other parts of the country.

In Rural Massachusetts, Patients and Physicians Weigh Trade-Offs of Concierge Medicine
Michele Andrews had been seeing her internist in Northampton, Massachusetts, a small city two hours west of Boston, for about 10 years. She was happy with the care, though she started to notice it was becoming harder to get an appointment. “You’d call and you’re […]
Health CareMichele Andrews had been seeing her internist in Northampton, Massachusetts, a small city two hours west of Boston, for about 10 years. She was happy with the care, though she started to notice it was becoming harder to get an appointment.
“You’d call and you’re talking about weeks to a month,” Andrews said.
That’s not surprising, as many workplace surveys show the supply of primary care doctors has fallen well below the demand, especially in rural areas such as western Massachusetts. But Andrews still wasn’t prepared for the letter that arrived last summer from her doctor, Christine Baker, at Pioneer Valley Internal Medicine.
“We are writing to inform you of an exciting change we will be making in our Internal Medicine Practice,” the letter read. “As of September 1st, 2024, we will be switching to Concierge Membership Practice.”
Concierge medicine is a business model in which a doctor charges patients a monthly or annual membership fee — even as the patients continue paying insurance premiums, copays, and deductibles. In exchange for the membership fee, doctors limit their number of patients.
Many physicians who’ve made the change said it resolved some of the pressures they faced in primary care, such as having too many patients to see in too short a time.
Andrews was floored when she got the letter. “The second paragraph tells me the yearly fee for joining will be $1,000 per year for existing patients. It’ll be $1,500 for new patients,” she said.
Although numbers are not tracked in any one place, the trade magazine Concierge Medicine Today estimates there are 7,000 to 22,000 concierge physicians in the U.S. Membership fees range from $1,000 to as high as $50,000 a year.
Critics say concierge medicine helps only patients who have extra money to spend on health care, while shrinking the supply of more traditional primary care practices in a community. It can particularly affect rural communities already experiencing a shortage of primary care options.
Andrews and her husband had three months to either join and pay the fee or leave the practice. They left.
“I’m insulted and I’m offended,” Andrews said. “I would never, never expect to have to pay more out of my pocket to get the kind of care that I should be getting with my insurance premiums.”
Baker, Andrews’ former physician, said fewer than half her patients opted to stay — shrinking her patient load from 1,700 to around 800, which she considers much more manageable. Baker said she had been feeling so stressed that she considered retiring.
“I knew some people would be very unhappy. I knew some would like it,” she said. “And a lot of people who didn’t sign up said, ‘I get why you’re doing it.’”
Patty Healey, another patient at Baker’s practice, said she didn’t consider leaving.
“I knew I had to pay,” Healey said. As a retired nurse, Healey knew about the shortages in primary care, and she was convinced that if she left, she’d have a very difficult time finding a new doctor. Healey was open to the idea that she might like the concierge model.
“It might be to my benefit, because maybe I’ll get earlier appointments and maybe I’ll be able to spend a longer period of time talking about my concerns,” she said.
This is the conundrum of concierge medicine, according to Michael Dill, director of workforce studies at the Association of American Medical Colleges. The quality of care may go up for those who can and do pay the fees, Dill said. “But that means fewer people have access,” he said. “So each time any physician makes that switch, it exacerbates the shortage.”
His association estimates the U.S. will face a shortage of 20,200 to 40,400 primary care doctors within the next decade.
A state analysis found that the percentage of residents in western Massachusetts who said they had a primary care provider was lower than in several other regions of the state.
Dill said the impact of concierge care is worse in rural areas, which often already experience physician shortages. “If even one or two make that switch, you’re going to feel it,” Dill said.
Rebecca Starr, an internist who specializes in geriatric care, recently started a concierge practice in Northampton.
For many years, she consulted for a medical group whose patients got only 15 minutes with a primary care doctor, “and that was hardly enough time to review medications, much less manage chronic conditions,” she said.
When Starr opened her own medical practice, she wanted to offer longer appointments — but still bring in enough revenue to make the business work.
“I did feel a little torn,” Starr said. While it was her dream to offer high-quality care in a small practice, she said, “I have to do it in a way that I have to charge people, in addition to what insurance is paying for.”
Starr said her fee is $3,600 a year, and her patient load will be capped at 200, much lower than the 1,000 or even 2,000 patients that some doctors have. But she still hasn’t hit her limit.
“Certainly there’s some people that would love to join and can’t join because they have limited income,” Starr said.

Many doctors making the switch to concierge medicine say the membership model is the only way to have the kind of personal relationships with patients that attracted them to the profession in the first place.
“It’s a way to practice self-preservation in this field that is punishing patients and doctors alike,” said internal medicine physician Shayne Taylor, who recently opened a practice offering “direct primary care” in Northampton. The direct primary care model is similar to concierge care in that it involves charging a recurring fee to patients, but direct care bypasses insurance companies altogether.
Taylor’s patients, capped at 300, pay her $225 a month for basic primary care visits — and they must have health insurance to cover care such as X-rays and medications, which her practice does not provide. But Taylor doesn’t accept insurance for any of her services, which saves her administrative costs.
“We get a lot of pushback because people are saying, ‘Oh, this is elitist, and this is only going to be accessible to people that have money,’” Taylor said.
But she said the traditional primary care model doesn’t work. “We cannot spend so much time seeing so many patients and documenting in such a way to get an extra $17 from the insurance company.”
While much of the pushback on the membership model comes from patients and policy experts, some of the resistance comes from physicians.
Paul Carlan, a primary care doctor who runs Valley Medical Group in western Massachusetts, said his practice is more stretched than ever. One reason is that the group’s clinics are absorbing some of the patients who have lost their doctor to concierge medicine.
“We all contribute through our tax dollars, which fund these training programs,” Carlan said.
“And so, to some degree, the folks who practice health care in our country are a public good,” Carlan said. “We should be worried when folks are making decisions about how to practice in ways that reduce their capacity to deliver that good back to the public.”
But Taylor, who has the direct primary care practice, said it’s not fair to demand that individual doctors take on the task of fixing a dysfunctional health care system.
“It’s either we do something like this,” Taylor said, “or we quit.”
This article is from a partnership that includes New England Public Media, NPR, and KFF Health News.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).

Alberta health officials warn of possible measles exposure in Calgary, Banff, Canmore
Alberta Health Services has issued a public alert about possible exposure to a confirmed case of measels in the communities of Calgary, Banff and Canmore.
MeaslesAlberta Health Services has issued a public alert about possible exposure to a confirmed case of measels in the communities of Calgary, Banff and Canmore.
Las familias de jóvenes trans ya no ven a Colorado como un refugio para la atención de afirmación de género
GRAND JUNCTION, Colorado — Un viernes después de la escuela, Esa Rodrigues, de 6 años, deshizo un ovillo de lana, asustó a su gato, preguntó a sus familiares sobre sus colores favoritos y delató a su hermano por llamarla “rata chismosa cara de trasero”. Luego, […]
Rural HealthGRAND JUNCTION, Colorado — Un viernes después de la escuela, Esa Rodrigues, de 6 años, deshizo un ovillo de lana, asustó a su gato, preguntó a sus familiares sobre sus colores favoritos y delató a su hermano por llamarla “rata chismosa cara de trasero”.
Luego, se concentró en abrir con los dientes un brillo labial con sabor a cereza.
“¡Sí!”, exclamó, cuando logró abrir la tapa. Esa se puso el brillo en su habitación, donde colgaba en la pared una gran bandera del orgullo transgénero.
Esa dijo que la bandera la hace sentir “importante” y “feliz”. Le gustaría quitarla de la pared y usarla como capa.
Al principio, sus padres cuestionaron su identidad, pero ya no. Antes, su hija, ansiosa, temía ir a la escuela, lloraba en la barbería cuando le hacían un corte “varonil”, y se acurrucó en posición fetal en el suelo del baño cuando supo que nunca tendría la menstruación.
Ahora, esa niña vive la vida con entusiasmo, preguntándose en voz alta si las hadas viven en la casita de cerámica que encontró encaramada en una piedra.
Su madre, Brittni Packard Rodrigues, quiere que esta alegría y aceptación perduren. Dependiendo de la combinación del deseo de Esa, las recomendaciones de sus médicos y el inicio de la pubertad, esto podría requerir bloqueadores, seguidos de estrógeno, para que Esa pueda desarrollar el cuerpo que se adapte a su ser.
“A largo plazo, los bloqueadores ayudan a prevenir todas esas cirugías y procedimientos que podrían convertirse en su realidad si no recibimos esa atención”, dijo Packard Rodrigues.
Los medicamentos conocidos como bloqueadores de la pubertad se usan ampliamente para afecciones como el cáncer de próstata, la endometriosis, la infertilidad y la pubertad precoz. Ahora, la administración Trump busca limitar su uso específicamente para jóvenes transgénero.
Colorado, el estado natal de Esa, es reconocido desde hace tiempo como un refugio para la atención de afirmación de género: se considera legalmente protegida y un beneficio esencial del seguro médico.
En los últimos años, “exiliados médicos” se han mudado a Colorado para recibir este tratamiento. Ya en la década de 1970, el pueblo de Trinidad se hizo conocida como “la capital mundial del cambio de sexo” cuando Stanley Biber, un ex cirujano del ejército con sombrero de vaquero, dejó su huella realizando estas cirugías en adultos.
En su primer día en el cargo, el presidente Donald Trump firmó una orden ejecutiva que refuta la existencia de personas transgénero, argumentando que es una “afirmación falsa que los hombres puedan identificarse como mujeres y, por lo tanto, convertirse en mujeres, y viceversa”.
A la semana siguiente, emitió otra orden que calificaba los bloqueadores de la pubertad y las hormonas para menores de 19 años como una forma de “mutilación” química y “una mancha en la historia de nuestra nación”. La orden instruía a las agencias a tomar medidas para garantizar que los beneficiarios de subvenciones federales para investigación o educación dejaran de proporcionarlos.
Organizaciones de atención médica en Colorado, California, Washington, D.C. y otros lugares anunciaron que cumplirían con la orden preventivamente.
En Colorado, esto incluía a tres importantes organizaciones de atención médica: Children’s Hospital Colorado, Denver Health y UCHealth.
Entre finales de enero y principios de febrero, los tres sistemas anunciaron cambios en la atención de afirmación de género que ofrecían a pacientes menores de 19 años, con efecto inmediato.
Dijeron que ya no recetarían nuevas hormonas ni bloqueadores de la pubertad para pacientes que no los hubieran recibido previamente, se limitarían o no se renovarían las recetas para quienes sí los hubieran recibido, y no se realizarían cirugías. Esto último aunque el Children’s Hospital nunca las había ofrecido, y este tipo de cirugía es poco común en adolescentes: por cada 100.000 menores trans, menos de tres se someten a ella.

El hospital infantil y Denver Health reanudaron la oferta de bloqueadores de la pubertad y hormonas el 24 y el 19 de febrero, respectivamente, después que Colorado se uniera a una demanda presentada ante el tribunal de distrito de EE. UU. en el estado de Washington.
El tribunal concluyó que las órdenes de Trump relacionadas con el género “discriminan por motivos de condición transgénero y sexo”. Otorgó una orden judicial preliminar que impide su entrada en vigencia en los cuatro estados involucrados.
Sin embargo, las cirugías no se han reanudado. Denver Health afirmó que “mantendrá la pausa en las cirugías de afirmación de género para pacientes menores de 19 años debido a la seguridad del paciente y dada la incertidumbre del panorama legal y regulatorio”.
UCHealth no ha reanudado ni la medicación ni la cirugía para menores de 19 años. “Nuestros proveedores esperan una decisión más definitiva de los tribunales federales que pueda resolver la incertidumbre en torno a la prestación de esta atención”, escribió la vocera Kelli Christensen.
Los jóvenes trans y sus familias afirmaron que el fallo judicial y las decisiones de los dos sistemas de salud de Colorado de reanudar los tratamientos no han resuelto el problema. Les ha dado tiempo para acumular recetas, para intentar encontrar médicos privados con la formación adecuada para supervisar los análisis de sangre, y ajustar las recetas en consecuencia, y, en algunos casos, para resolver la logística de mudarse a otro estado o país.
La administración Trump ha seguido presionando a los proveedores de salud más allá de las órdenes ejecutivas iniciales, amenazando con retener o cancelar los fondos federales que se les habían otorgado. A principios de marzo, la Administración de Recursos y Servicios de Salud (RHSA) anunció que revisaría la financiación de la educación médica de posgrado en hospitales pediátricos.
KFF Health News solicitó comentarios a Kush Desai, subsecretario de prensa de la Casa Blanca, pero no recibió respuesta. La subsecretaria de prensa del Departamento de Salud y Servicios Sociales (HHS), Emily Hilliard, respondió con enlaces a dos comunicados de prensa anteriores.

Las intervenciones médicas son solo un tipo de atención de afirmación de género, y el proceso para obtener el tratamiento es largo y exhaustivo.
Investigadores han descubierto que, incluso entre quienes tienen seguro médico privado, es poco probable que los jóvenes transgénero reciban bloqueadores de la pubertad ni hormonas. Curiosamente, la mayoría de las cirugías de reducción de senos para afirmación de género realizadas en hombres y menores se practican en pacientes cisgénero, no transgénero.
Kai, de 14 años, quisiera haber podido tomar bloqueadores de la pubertad. Vive en Centennial, un suburbio de Denver. KFF Health News no divulga su nombre completo porque a su familia le preocupa que pueda sufrir acoso.
Kai tuvo su primera menstruación a los 8 años. Para el momento en el que se dio cuenta de que era transgénero, en la secundaria, ya era demasiado tarde para empezar a tomar bloqueadores de la pubertad.
Sus médicos le recetaron anticonceptivos para suprimir sus períodos, así no le recordaban cada mes su disforia de género. Luego, al cumplir los 14, empezó a tomar testosterona.
Kai dijo que si no estuviera en terapia hormonal ahora, sería un peligro para sí mismo.
“Poder decir que estoy feliz con mi cuerpo y poder ser feliz en público sin pensar que todos me miran raro, es una gran diferencia”, dijo.
Su madre, Sherry, dijo que se alegra de ver a Kai relajarse y convertirse en la persona que es.
Sherry, quien pidió usar su segundo nombre para evitar que se identificara a su familia, dijo que comenzó a guardar testosterona en cuanto Trump fue elegido, pero no había pensado en el impacto que esto tendría en la disponibilidad de anticonceptivos. Sin embargo, después de las órdenes ejecutivas, esa receta también se volvió difícil de conseguir. Sherry dijo que el médico de Kai en UCHealth tuvo que programar una reunión especial para confirmar que podía seguir recetándosela.
Así que, por ahora, Kai tiene lo que necesita. Pero para Sherry, eso no es un gran consuelo.
“No creo que estemos muy seguros”, dijo. “Son solo prórrogas”.
La familia está ideando un plan para salir del país. Si Sherry y su esposo consiguen trabajo en Nueva Zelanda, se mudarán allí. Sherry dijo que esa posibilidad es un privilegio que muchos otros no tienen.
Por ejemplo, David, un estudiante de 18 años de la Universidad Western Colorado en Gunnison, un pueblo de las Montañas Rocallosas, pidió ser identificado solo por su segundo nombre porque le preocupa ser objeto de persecución en este pueblo rural y conservador.
David no tiene pasaporte, pero incluso si lo tuviera, no quiere irse de Gunnison, dijo. Está estudiando geología y aprendiendo a tocar el bajo.
Y tiene un buen grupo de amigos. Planea ser paleontólogo.
Los estantes de su dormitorio están llenos de sus artículos esenciales: fósiles, desodorante Old Spice, macarrones con queso para microondas. Pero no hay espejos. David dijo que se acostumbró a evitarlos.
“Durante mucho tiempo, tuve tanta disforia corporal y dismorfia que puede ser un poco difícil mirarme al espejo”, dijo David. “Pero cuando lo hago, la mayoría de las veces, veo algo que realmente me gusta”.
Lleva tres años tomando testosterona, y la hormona le ayudó a que creciera su barba. En enero, le dijeron a su médico de Denver Health que dejara de recetársela. Su madre condujo horas desde su casa hasta Gunnison para darle la noticia en persona.
La receta ya está activa de nuevo, pero la mastectomía que había planeado para este verano no. Esperaba tener un tiempo de recuperación adecuado antes de empezar el segundo año de la universidad. Pero no conoce a nadie en Colorado que lo haga antes de los 19 años. Podría operarse fácilmente para aumentar sus pechos, pero debe buscar opciones quirúrgicas en otros estados para reducirlos o extirparlos.
“Se suponía que Colorado, como estado, era un refugio”, dijo su madre, Louise, quien pidió ser identificada por su segundo nombre. “Tenemos una ley que otorga a las personas trans el derecho a la atención médica, y sin embargo, nuestros sistemas de salud se la están quitando”.
Han sido necesarios ocho años y unos diez profesionales médicos y terapeutas para que David esté tan cerca de la meta. Es un gran logro después de haber vivido tantos años de disforia y dismorfia.
“Sigo adelante, y seguiré adelante, y casi nada podrá detenerme, porque así soy”, dijo David. “Siempre ha habido personas trans y siempre las habrá”.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).

Deportation Fears Add to Mental Health Problems Confronting Colorado Resort Town Workers
SILVERTHORNE, Colo. — When Adolfo Román García-Ramírez walks home in the evening from his shift at a grocery store in this central Colorado mountain town, sometimes he thinks back on his childhood in Nicaragua. Adults, he recollects, would scare the kids with tales of the […]
Rural HealthSILVERTHORNE, Colo. — When Adolfo Román García-Ramírez walks home in the evening from his shift at a grocery store in this central Colorado mountain town, sometimes he thinks back on his childhood in Nicaragua. Adults, he recollects, would scare the kids with tales of the “Mona Bruja,” or “Monkey Witch.” Step too far into the dark, they told him, and you might just get snatched up by the giant monstrous monkey who lives in the shadows.
Now, when García-Ramírez looks over his shoulder, it’s not monster monkeys he is afraid of. It’s U.S. Immigration and Customs Enforcement officers.
“There’s this constant fear that you’ll be walking down the street and a vehicle rolls up,” García-Ramírez, 57, said in Spanish. “They tell you, ‘We’re from ICE; you’re arrested,’ or, ‘Show me your papers.’”
Silverthorne, a commuter town between the ski meccas of Breckenridge and Vail, has been García-Ramírez’s home for the past two years. He works as a cashier at the grocery and shares a two-bedroom apartment with four roommates.
The town of nearly 5,000 has proved a welcome haven for the political exile, who was released from prison in 2023 after Nicaragua’s authoritarian government brokered a deal with the U.S. government to transfer more than 200 political prisoners to the U.S. The exiles were offered temporary residency in the U.S. under a Biden administration humanitarian parole program.
García-Ramírez’s two-year humanitarian parole expired in February, just a few weeks after President Donald Trump issued an executive order to end the program that had permitted temporary legal residency in the U.S. for hundreds of thousands of Cubans, Haitians, Nicaraguans, and Venezuelans, putting him at risk of deportation. García-Ramírez was stripped of his Nicaraguan citizenship when he came to the U.S. Just over a year ago, he applied for political asylum. He is still waiting for an interview.
“I can’t safely say I’m calm, or I’m OK, right now,” García-Ramírez said. “You feel unsafe, but you also feel incapable of doing anything to make it better.”
Vail and Breckenridge are world famous for their ski slopes, which attract millions of people a year. But life for the tourism labor force that serves Colorado’s mountain resorts is less glamorous. Residents of Colorado’s mountain towns experience high rates of suicide and substance use disorders, fueled in part by seasonal fluctuations in income that can cause stress for many in the local workforce.
The Latino communities who make up significant proportions of year-round populations in Colorado’s mountain towns are particularly vulnerable. A recent poll found more than 4 in 5 Latino respondents in the Western Slope region, home to many of the state’s rural ski resort communities, expressed “extremely or very serious” concern about substance use. That’s significantly higher than in rural eastern Colorado’s Morgan County, which also has a sizable Latino population, and in Denver and Colorado Springs.
Statewide, concerns about mental health have surged among Latinos in recent years, rising from fewer than half calling it an extremely or very serious problem in 2020 to more than three-quarters in 2023. Health care workers, researchers, and community members all say factors such as language differences, cultural stigma, and socioeconomic barriers may exacerbate mental health issues and limit the ability to access care.
“You’re not getting regular medical care. You’re working long hours, which probably means that you can’t take care of your own health,” said Asad Asad, a Stanford University assistant professor of sociology. “All of these factors compound the stresses that we all might experience in daily life.”
Add sky-high costs of living and an inadequate supply of mental health facilities across Colorado’s rural tourist destinations, and the problem becomes acute.
Now, the Trump administration’s threats of immigration raids and imminent deportation of anyone without legal U.S. residency have caused stress levels to soar. In communities around Vail, advocates estimate, a vast majority of Latino residents do not have legal status. Communities near Vail and Breckenridge have not experienced immigration raids, but in neighboring Routt County, home to Steamboat Springs, at least three people with criminal records have been detained by ICE, according to news reports. Social media posts falsely claiming local ICE sightings have further fueled concerns.
Yirka Díaz Platt, a bilingual social worker in Silverthorne originally from Peru, said a pervasive fear of deportation has caused many Latino workers and residents to retreat into the shadows. People have begun to cancel in-person meetings and avoid applying for government services that require submitting personal data, according to local health workers and advocates. In early February, some locals didn’t show up to work as part of a nationwide “day without immigrants” strike. Employers wonder whether they will lose valuable employees to deportation.
Some immigrants have stopped driving out of fear they will be pulled over by police. Paige Baker-Braxton, director of outpatient behavioral health at the Vail Health system, said she has seen a decline in visits from Spanish-speaking patients over the last few months.
“They’re really trying to keep to themselves. They are not really socializing much. If you go to the grocery stores, you don’t see much of our community out there anymore,” Platt said. “There’s that fear of, ‘No, I’m not trusting anyone right now.’”
Juana Amaya is no stranger to digging in her heels to survive. Amaya immigrated to the Vail area from Honduras in 1983 as a single mother of a 3-year-old and a 6-month-old. She has spent more than 40 years working as a house cleaner in luxury condos and homes around Vail, sometimes working up to 16 hours a day. With barely enough time to finish work and care for a family at home, she said, it is often hard for Latinos in her community to admit when the stress has become too much.
“We don’t like to talk about how we’re feeling,” she said in Spanish, “so we don’t realize that we’re dealing with a mental health problem.”
The current political climate has only made things worse.
“It’s had a big impact,” she said. “There are people who have small children and wonder what they’ll do if they’re in school and they are taken away somewhere, but the children stay. What do you do?”
Asad has studied the mental health impacts of deportation rhetoric on Latino communities. He co-authored a study, published last year in the journal Proceedings of the National Academy of Sciences, that found escalated deportation rhetoric may cause heightened levels of psychological distress in Latino noncitizens and even in Latino citizens.
Asad found that both groups may experience increased stress levels, and research has borne out the negative consequences of a parent’s lack of documentation on the health and educational attainment of their children.
“The inequalities or the hardships we impose on their parents today are the hardships or inequalities their children inherit tomorrow,” Asad said.
Despite heightened levels of fear and anxiety, Latinos living and working near Vail still find ways to support one another and seek help. Support groups in Summit County, home to Breckenridge and less than an hour’s drive from Vail, have offered mental health workshops for new immigrants and Latina women. Building Hope Summit County and Olivia’s Fund in Eagle County, home to Vail, help those without insurance pay for a set number of therapy sessions.
Vail Health plans to open a regional inpatient psychiatric facility in May, and the Mobile Intercultural Resource Alliance provides wraparound services, including behavioral health resources, directly to communities near Vail.
Back in Silverthorne, García-Ramírez, the Nicaraguan exile, takes things one day at a time.
“If they deport me from here, I’d go directly to Nicaragua,” said García-Ramírez, who said he had received a verbal death threat from authorities in his native country. “Honestly, I don’t think I would last even a day.”
In the meantime, he continues to make the routine trek home from his cashier job, sometimes navigating slick snow and dark streets past 9 p.m. When nightmarish thoughts about his own fate in America surface, García-Ramírez focuses on the ground beneath his feet.
“Come rain, shine, or snow,” he said, “I walk.”
This article was published with the support of the Journalism & Women Symposium (JAWS) Health Journalism Fellowship, assisted by grants from The Commonwealth Fund.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).

States Push Medicaid Work Rules, but Few Programs Help Enrollees Find Jobs
For many years, Eric Wunderlin’s health issues made it hard to find stable employment. Struggling to manage depression and diabetes, Wunderlin worked part-time, minimum-wage retail jobs around Dayton, Ohio, making so little he said he sometimes had to choose between paying rent and buying food. […]
Health CareFor many years, Eric Wunderlin’s health issues made it hard to find stable employment.
Struggling to manage depression and diabetes, Wunderlin worked part-time, minimum-wage retail jobs around Dayton, Ohio, making so little he said he sometimes had to choose between paying rent and buying food.
But in 2018, his CareSource Medicaid health plan offered him help getting a job. It connected him to a life coach, who helped him find full-time work with health benefits. Now, he works for a nonprofit social service agency, a job he said has given him enough financial stability to plan a European vacation next year.
“I feel like a real person and I can go do things,” said Wunderlin, 42. “I feel like I pulled myself out of that slump.”
Republicans in Congress and several states, including Ohio, Iowa, and Montana, are pushing to implement work requirements for nondisabled adults, arguing a mandate would encourage enrollees to find jobs. And for Republicans pushing to require Medicaid enrollees to work, Wunderlin’s story could be held up as evidence that government health coverage can help people find employment and, ultimately, reduce their need for public assistance.
Yet his experience is rare. Medicaid typically does not offer such help, and when states do try to help, such efforts are limited.
And opponents point out that most Medicaid recipients already have jobs and say such a mandate would only kick eligible people off Medicaid, rather than improve their economic prospects. Nearly two-thirds of Medicaid enrollees work, with most of the rest acting as caregivers, going to school, or unable to hold a job due to disability or illness, according to KFF, a health information nonprofit that includes KFF Health News.
Existing efforts to help Medicaid recipients get a job have seen limited success because there’s not a lot of “room to move the needle,” said Ben Sommers, a professor of health care economics at the Harvard T.H. Chan School of Public Health. Most Medicaid enrollees already work — just not in jobs with health benefits, he said.
“The ongoing argument that some folks make is that there are a lot of people freeloading in Medicaid,” he said. “That’s just not supported by the evidence.”

Using Health Programs To Encourage Work
The GOP-controlled Congress could allow or require states to implement a Medicaid work requirement as part of revamping and downsizing Medicaid. The first Trump administration encouraged those work mandates, but many were struck down by federal judges who said they were illegal under federal law.
Policy experts and state officials say more attention should be paid to investments that have helped people find better jobs — from personalized life coaching to, in some cases, health plans’ directly hiring enrollees.
They argue work requirements alone are not enough. “The move to economic mobility requires a ladder, not a stick,” said Farah Khan, a fellow with the Brookings Institution, a nonpartisan think tank.
While Medicaid work requirements have been debated for decades, the issue has become more heated as 40 states and Washington, D.C., have expanded Medicaid eligibility under the Affordable Care Act to the vast majority of low-income adults. More than 20 million adults have gained coverage as a result — but Republicans are now considering eliminating the billions in extra federal funding that helped states extend eligibility beyond groups including many children, pregnant women, and disabled people.
Only Georgia and Arkansas have implemented mandates that some Medicaid enrollees work, volunteer, go to school, or enroll in job training. But a study Sommers co-authored showed no evidence work requirements in Arkansas’ program led to more people working, in part because most of those who could work already were.
In Arkansas, more than 18,000 people lost coverage under the state’s requirement before the policy was suspended by a federal judge in 2019 after less than a year. Those who lost their Medicaid health care reported being unaware or confused about how to report work hours. Since 2023, Arkansas has been giving Medicaid health plans financial incentives to help enrollees train for jobs, but so far few have taken advantage.
Some plans, including Arkansas Blue Cross and Blue Shield’s, offer members $25 to $65 to complete a “career readiness” certificate. In 2024, some Arkansas health plans offered enrollees educational videos about topics including taxes and cryptocurrency.
Health plans don’t have an incentive to help someone find a better-paying job, because that could mean losing a customer if they then make too much to qualify for Medicaid, said Karin VanZant, a vice president at Clearlink Partners, a health care consulting company.
Rather than offering incentives for providing job training, some states, such as California and Ohio, require the insurance companies that run Medicaid to help enrollees find work.
In Montana, where some lawmakers are pushing to implement work requirements, a promising optional program nearly collapsed after state lawmakers required it be outsourced to private contractors.
Within the program’s first three years, the state paired 32,000 Medicaid enrollees with existing federally funded job training programs. Most had higher wages a year after starting training, the state found.
But enrollment has plummeted to just 11 people, according to the latest data provided by the state’s labor department.
Sarah Swanson, who heads the department, said several of the nonprofit contractors that ran the program shuttered. “There was no real part in this for us to deliver direct services to the folks that walked through our door,” she said. The state hopes to revive job training by allowing the department to work alongside contractors to reach more people.
More from Medicaid Watch
-

The House Speaker’s Eyeing Big Cuts to Medicaid. In His Louisiana District, It’s a Lifeline.
Apr 7, 2025
-

‘If They Cut Too Much, People Will Die’: Health Coalition Pushes GOP on Medicaid Funding
Apr 3, 2025
-

Many People With Disabilities Risk Losing Their Medicaid if They Work Too Much
Mar 25, 2025
The Hunt for Results
State officials say they don’t have much data to track the effectiveness of existing job programs offered by Medicaid plans.
Stephanie O’Grady, a spokesperson for the Ohio Department of Medicaid, said the state does not track outcomes because “the health plans are not employment agencies.”
Officials with CareSource, which operates Medicaid plans in multiple states, say it has about 2,300 Medicaid and ACA marketplace enrollees in its JobConnect program — about 1,400 in Ohio, 500 in Georgia, and 400 in Indiana.
The program connects job seekers with a life coach who counsels them on skills such as “showing up on time, dressing the part for interviews, and selling yourself during the interview,” said Jesse Reed, CareSource’s director of life services in Ohio.


Since 2023, about 800 people have found jobs through the program, according to Josh Boynton, a senior vice president at CareSource. The health plan itself has hired 29 Medicaid enrollees into customer service, pharmacy, and other positions — nearly all full-time with benefits, he said.
In 2022, California started offering nontraditional health benefits through Medicaid — including help finding jobs — for enrollees experiencing homelessness or serious mental illness, or who are otherwise at risk of avoidable emergency room care. As of September, it had served nearly 280,000 enrollees, but the state doesn’t have data on how many became employed.
The University of Pittsburgh Medical Center, which is among the largest private employers in Pennsylvania, running both a sprawling hospital system and a Medicaid plan, has hired over 10,000 of its Medicaid enrollees since 2021 through its training and support services. Among other jobs, they took positions as warehouse workers, customer service representatives, and medical assistants.
The vast majority left low-paying jobs for full-time positions with health benefits, said Dan LaVallee, a senior director of UPMC Health Plan’s Center for Social Impact. “Our Pathways to Work program is a model for the nation,” he said.
Josh Archambault, a senior fellow with the conservative Cicero Institute, said Medicaid should focus on improving the financial health of those enrolled.
While the first Trump administration approved Medicaid work requirements in 13 states, the Biden administration or federal judges blocked all except Georgia’s.
“I don’t think states have been given ample chance to experiment and try to figure out what works,” Archambault said.
KFF Health News senior correspondent Angela Hart contributed to this report.
KFF Health News is a national newsroom that produces in-depth journalism about health issues and is one of the core operating programs at KFF—an independent source of health policy research, polling, and journalism. Learn more about KFF.
USE OUR CONTENT
This story can be republished for free (details).